Varicose Veins Treatment in Joplin, MO
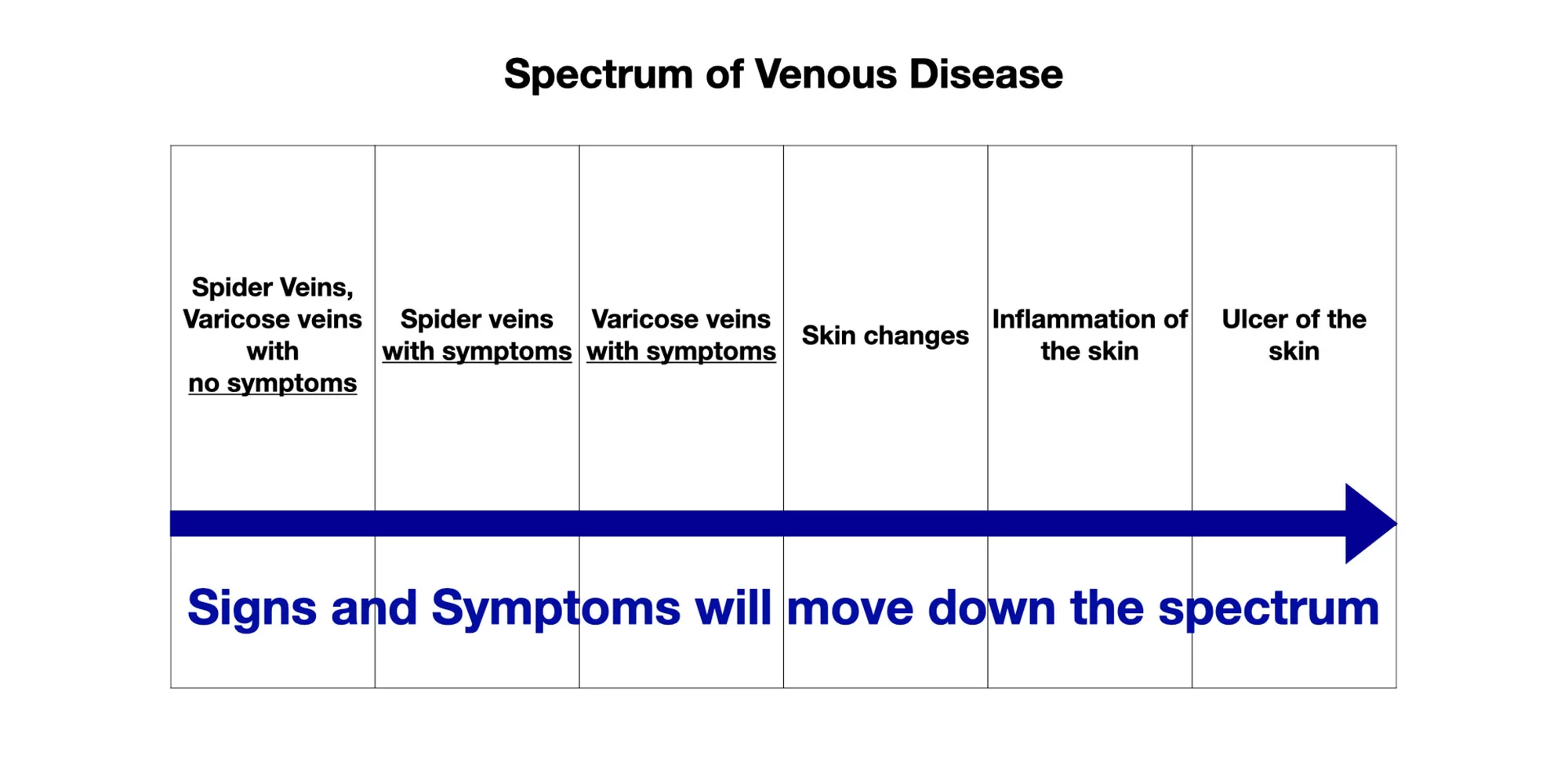
Venous disease exists on a spectrum and can present with a variety of signs and symptoms. One of the most common conditions is varicose veins—veins located just beneath the skin that have become enlarged and visibly dilated.
Varicose veins develop when the valves within the leg veins, which normally help blood flow upward toward the heart, stop working efficiently. Instead of moving out of the leg, blood flows backward, creating increased pressure within the main and branch veins. This backflow leads to venous congestion, which can cause visible bulging veins, discomfort, and other complications if left untreated.
Can I have treatment for my venous disease?
Yes. Most treatments for venous disease can be performed under local anesthetic or with light sedation to ensure comfort. For patients with higher anxiety or additional health concerns, heavier anesthesia may be used for safety. Age is not a barrier to treatment—Dr. Warren Albrecht has successfully treated patients ranging from their 20s to their 90s. Only a very small percentage of individuals are not candidates for therapy.
How Common Is Venous Disease?
Venous disease is extremely common—more prevalent in the United States than coronary artery disease, peripheral arterial disease, congestive heart failure, and stroke combined.
- In 2011, the Society for Vascular Surgery and the American Venous Forum published guidelines for the treatment of chronic venous disease and varicose veins.
- At that time, an estimated 23% of adults had varicose veins and 6% had more advanced chronic venous disease (including skin changes, inflammation, or ulcers).
- Applied to today’s population, that equals approximately 69 million Americans with varicose veins and 18 million with advanced venous disease.
What Causes Varicose Veins?
The anatomical cause of venous disease is well understood: malfunctioning vein valves that allow blood to pool and flow backward. However, three consistent risk factors increase the likelihood of developing varicose veins:
- Two or more pregnancies
- Heredity or family history
- A lifestyle that involves prolonged standing or sitting
Signs of Venous Disease:
Venous disease may present with or without visible varicose veins. Common signs include:
- Prominent veins above the feet, ankles, calves, or thighs
- Darkened or pigmented skin around the calves due to venous congestion
- Lipodermatosclerosis – changes in the skin of the lower legs, including inflammation of the fat layer causing pain, skin hardening, redness (not infection), swelling, and tapering above the ankles
- Current or past open skin wounds or ulcers
Symptoms of Venous Disease:
- Aching or pain
- Burning sensations
- Leg tightness or heaviness
- Swelling
- Skin irritation or itching
- Tiredness or fatigue
- Muscle cramps
Varicose Veins are a Varicose Veins: A Spectrum of One Disease
Varicose veins and venous disease exist on a spectrum, ranging from small, harmless-appearing spider veins to more serious complications. Signs and symptoms can include:
- Tiny spider veins
- Enlarged, worm-like veins without symptoms
- Aching or discomfort in the legs
- Swelling and fluid buildup
- Darkening or discoloration of the skin
- Skin inflammation
- Bleeding veins or infections
- Open sores, also known as venous ulcers
All of these conditions stem from venous hypertension—back pressure caused when vein valves fail and blood flows backward. This backward pressure leads to fluid accumulation, swelling, and stretching of the veins, resulting in visible skin changes and varicose veins.
It’s important to understand that patients can “skip” stages of the disease. Many people live with varicose veins for years without problems, only to suddenly develop complications such as skin infections or ulcers. These advanced cases are often seen in the wound care clinic, highlighting the importance of early evaluation and treatment.

Does my medical insurance pay for treatment?
- Medical insurance will want an ultrasound which we can provide at Mercy.
- Medical insurance will require usually three months of a trial of compression stockings during the day at work. This will not include the nighttime or weekends.
References of above information: https://www.venousforum.org/resources/guidelines/